|
“Smile, breathe, and go slowly.” – Thich Nhat Hanh
Interested in learning a bit about perinatal anxiety - or anxiety in pregnancy and the postpartum period? I created a Facebook Live introductory video. Grab a warm cup of tea and learn a bit about what's happening and how to respond! Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. Too often we underestimate the power of a touch, a smile, a kind word, a listening ear, an honest compliment, or the smallest act of caring, all of which have the potential to turn a life around. -Leo Buscaglia
The reason for recommending groups for perinatal support is simple: We need each other. This whole “it takes a village” thing is not just a cliche. It’s an epic Truth. When we were near and with one another, we SAW what pregnancy and postpartum life was like. We witnessed the hard parts, the joyous parts, the mundane parts, and we took care of each other in big and small ways. These days, in this culture there’s a lot more individualism and with that isolation and loneliness. Being in a group of moms and sharing honest experience can help reduce some of that. Here are some San Francisco groups you can count on to be there for you. Since I have the pleasure of knowing some of the providers, I asked them to shared just a touch of their own reasons for providing these groups. CPMC Newborn Connections. CPMC offers two weekly 90-minute drop-in groups, one for moms of babies age 0-3 months and another for those with babes 3+ months. In each, members can connect about the joys and anxieties of new parenthood (and everything between). The cost is $5 and you don’t have to be a patient of CPMC's to attend. Brett Collins, the former facilitator says, "Your village is waiting! Come as you are - there's no such thing as late and everyone is welcome to cry (babies and parents)." (Laurel Heights) Natural Resources: Natural resources offers two weekly hour-long, drop-in baby support groups, for parents of babies 0-3 months and 3+ months, respectively. "It is a place to share about whatever is on your heart and mind surrounding parenting - and is an opportunity to meet other new parents and form lasting friendships. Babies are welcome"! The cost for members is $10, $15 for non-members. While you’re there you can peruse all their baby gear, talk to their welcoming and helpful staff (who know a lot about said baby gear) and check out their other offerings, which include lactation support, classes, and a host of other support and educational groups. (Mission District) Postpartum SF: Postpartum SF is made up of two clinicians who have come together to provide support groups to those having emotional wellness challenges in new parenthood. It covers relationship changes, attachment to baby, self-care, identity shifts and more. The group is capped at 7 members at a time and runs on an 8-week cycle, repeating throughout the year. This group is designed to occur without babies present in order to give more focused attention to members. The current rate is $480 for the series which breaks down to $60 per 90-minute session. They ask that women commit to all 8-sessions but they can pay either up front, weekly, or monthly - whatever works best for them. The facilitators, Katy Lonergan and Alexis Monnier created the group because "We believe all moms struggle in some fashion and we want them to know they aren't alone.” (Lower Pacific Heights) Recess: Facilitated by an infant mental health specialist, Recess hosts an hour-long new parents meet-up for expectant parents and those with babies under the age of one. In this group you’ll organically meet like-minded parents and begin building your new family’s community, while gaining resources to help support your little one's growth. Guest speakers relevant to your baby's needs will drop by with specialized areas of focus like sleeping, eating, and self-care. Suggested donation is $15 and no one is turned away for lack of funds. As for the “why”behind the group, Lisa G, owner of Recess shares, "The first year of parenting is such a rollercoaster. We want to give new parents a space they can show up, in any state, and just be. They can share or just absorb, connect with others or connect with their babe. Our goal is to meet each mama and papa where they are and provide support." (Potrero Hill) UCSF - The Afterglow: The Afterglow is a 6-week group that repeats throughout the year, and is for moms of babies 0-6 months old who are UCSF patients. I gotta tell you, I've only heard glowing reviews of this group (pun intended), where you'll learn, discuss, and connect with others, in addition to practicing some new self-care strategies. It's $150 for the series with limited sliding scale slots available, and is facilitated by two dedicated mama supports, Juli Fraga and Melissa Whippo. Their reason for providing the group? "We’d love moms to know they are not alone and that we need to b able to speak our truths about the full motherhood experience" (Mission Bay) So there's a start mama (mama-to-be, or someone who's keeping a caring eye out)! You can always reach out to the facilitators for more info. You will be lovingly received. Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. It's Maternal Mental Health Month - a time for bringing light to the facets of motherhood oft left in the dark - including the messy, hard parts, and those involving perinatal mood and anxiety disorders (PMADS).
As such I'll be doing a few Facebook lives to do my part in demystifying some mental health related topics, such as perinatal anxiety and depression, and highlighting a ton of resources that can be helpful during early parenthood. I hope you find something directly helpful to you and I sure do hope you share with a mom or mom-to-be who you care about. We're all stronger together. Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. I think we all know that disappointed, helpless feeling when the thing we need the most feels out of reach (I feel mine in the pit of my stomach). That's the shared experience we'll touch on today in the context of connecting with partner through new parenthood.
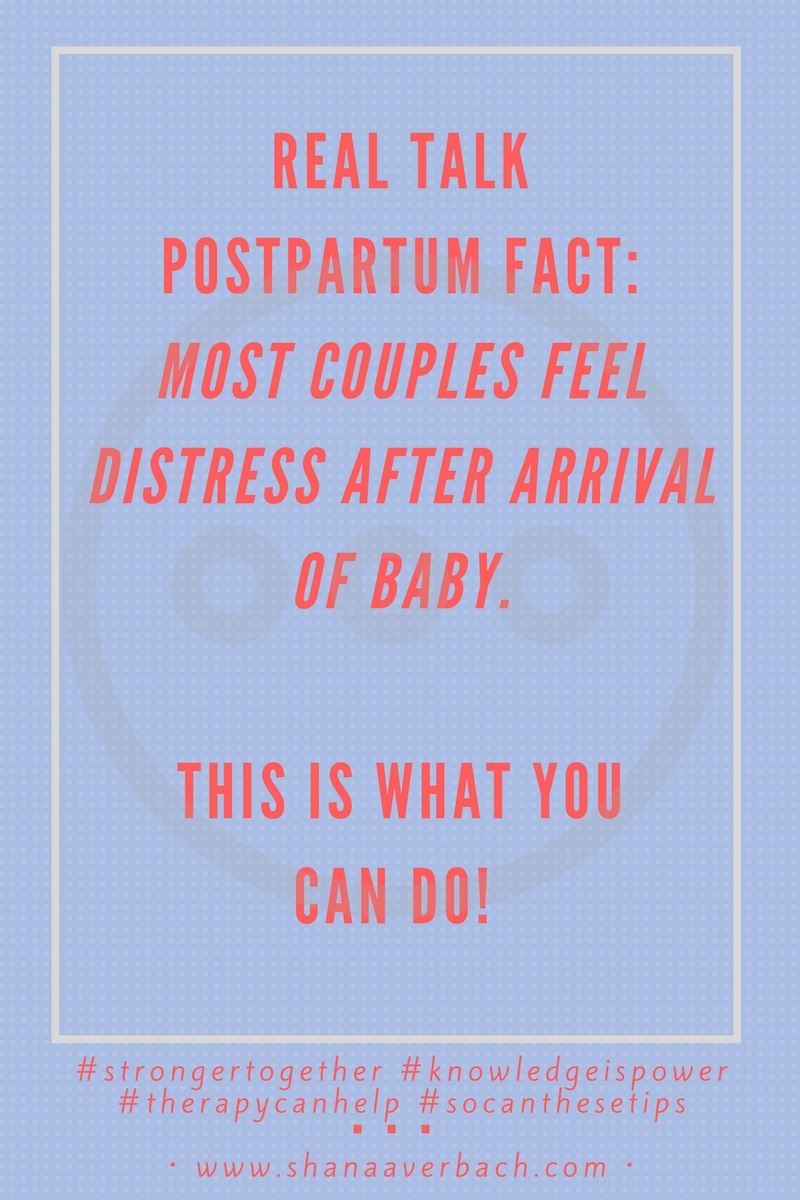
If you're finding yourself here for the first time welcome. You can read more about this passion project here and get this content straight to your inbox here. Today I'll share the next batch of feedback from the survey, along with some more resources and words of wisdom from a few therapist colleagues. This time we're focusing on the subject of postpartum relationship woes, specifically feelings of disconnection from partner. First a touch of research on the topic: According to the Gottmans, the husband-wife team from the Gottman Institute and the The Relationship Research Institute in Seattle, Washington (and authors of the Book And Baby Makes Three, which is an excellent resource in and of itself), in studying 130 families long-term: “[I]n the first three years after babies were born a whopping two-thirds of parents experienced a significant drop in their relationship quality" (p. 16). The Gottmans actually indicate research from the 1950s and 1980s that have the the numbers at more like 80-something percent. That's a lot of distressed couples. I recalled these statistics when I saw our numbers from the survey, because what do you know? Of our 200+ sample, about 62% of respondents indicated this experience postpartum (which was a big leap from the 26% of moms who felt this disconnection during pregnancy). This number is high enough, but it was highlighted further by the fact that the majority of our moms - nearly 77% - when asked with whom they shared their big feelings (you know, the anxiety, sad thoughts, along with the joys, etc.), indicated their partners. Think about that for a sec. This means that mamas are sharing their most personal, nuanced, sometimes scary thoughts and feelings with their partners, and feeling like they can't quite access them at the same time. Ugh. What could possibly be happening here? Let's start with the common sense approach: Why wouldn't it be tough on a relationship to bring a brand new person into the equation, much less one who is completely dependent on you? Why wouldn't your primary relationship be strained against the backdrop of sleep deprivation, a million new tasks, and, in all likelihood, minimal additional support? And who do you know who's at their personal and relational best when staring up a mountain of I-don't-know-how-to-do-this-ness (and by the way you cannot for the life of you see the peak, so have no idea how long the climb). When we think about it this way, some of the tension can be mitigated by adjusting expectations. But that's not enough. Cause this becoming a parent shit is hard, and the voice of reason is easily drowned by the cries of all of the above. Since I work largely with individuals, I asked some passionately couples-focused members of my therapist tribe to share their thoughts on this, specifically,
According to Christie Sears Thompson, MA, MFTC (www.tradewindstherapy.com), who practices in Wheat Ridge, CO, “Exhaustion as well as lack of self-care and relationship-care are pretty big barriers to connection. Many couples are in survival mode after their baby is born. Not only are they sleep deprived, but they are trying to manage life around the demands of a tiny human. When a baby is introduced to new parents, typically the focus of care shifts in that direction. Each partner's self-care usually takes a huge step backwards and relationship-care sometimes becomes non-existent. New parents have to implement self-care. I teach my clients about the eight facets of self-care: emotional, physical, nutritional, relational, spiritual, sensual, contextual, and intellectual. We review each of these categories and discuss how each person can address these areas more effectively. I find that when my clients can manage better self-care practices, they feel better overall and it becomes much easier to connect with their partner and reinstate some healthy relationship-care practices.” Jessica Cowling, LCSW (www.jessicacowling.com) in London Ontario Canada says this: “I see that most new parents don't understand each other's stress. Dad doesn't understand how busy it is looking after a baby all day, and how emotionally draining it is, and how much she doesn't want to be touched, and how desperate she is for adult interaction. Mom doesn't understand that Dad is tired too (although probably not as tired as her!), that he feels an enormous amount of pressure to provide for the family, that he too is probably craving some alone time when he gets home from work, that he might feel quite inadequate and/or useless when it comes to looking after baby, especially if Mom doesn't let him do anything with the baby or takes over when he does it "wrong". And competition/scorekeeping. The short answer is that they are probably just not aware of and prepared for the changes that are coming. I tend to use Emotionally Focused Therapy (Sue Johnson), so we talk a lot about the negative cycles of interaction. Often it's just making space for them to express their frustrations, and helping the other to hear and understand. And normalizing their experience.” According to Sarah Tie, NC, LPCC (www.windingpathcounseling.com) in Denver, CO , “One of the biggest obstacles that I encounter is the belief that the child always has to come first.” [The authors of this article agree!] When a couple first has a baby their focus and attention automatically shifts to the baby. While this makes sense for a while, I find that after the adjustment period has passed, many parent struggle to pull focus back onto themselves and let go of the guilt that comes from taking time away from their child. The message that I give all parents about this is: when you and your partner are healthy and happy, your child is getting the best from you both. In other words, by taking some time for you, you are actually doing what is also in the best interests of your kid: giving him or her happy parents. To this end, I always recommend planning regular dates or time off, whether or not you have something planned. Have regular time set aside for you and your partner - make it a habit, because spontaneity isn’t an option when you have a small child”! And finally, *Nicole O'Conner, LMFT, ATR (http://www.nicoleoconnormft.com/) in San Francisco, CA notices this: “Each family is different, but generally speaking: management of basic needs (sleeping, eating, using the bathroom/showering), lack of social support, Increase in defensiveness and criticism between the couple due to stress, worry that it will always be this difficult Come up with a plan for basic needs (i.e., sleeping in shifts, schedule meals and showers, etc). This helps to reduce resentment, so the couple can connect with each other around the love of their new baby. Having the non-feeding partner step in and start doing household chores without being asked, helping to reduce worry and increase emotional space for the appreciation. Find support systems outside the marriage - parents groups, moms groups, online neighborhood parents groups. Work on finding other parents that you enjoy having a cup of coffee with to help reduce the expectation that the partner will be all things. Be mindful in the moment to not criticize and/or defend yourself, if one person is winning then you're both losing. Remember that most couples have a "perpetual problem" that continues to come up over and over, the problem is not in the other person, but rather how you dialogue about that issue.” *For our local SF mamas, Nicole O'Connor will be conducting a couples workshop on July 15th and again on September 30th at Natural Resources. For more information visit: https://www.naturalresources-sf.com/products/transitioning-from-partners-to-parents To summarize so far, in the face of relational distress and disconnection, which the majority of new parents feel, we can:
For those of you wanting more structure and facilitation, here are some more resources options, Remember the Gottmans? Well they used their research to create workshops which are held across the map. Check out their offerings here. https://www.gottman.com/parents/ Another option is Elly Taylor's work, which focuses specifically on the adventure into parenthood. She has an 8-step book and is training therapists to facilitate:https://ellytaylor.com/parenthood-1 And last but anything but least, Dr. Sue Johnson the founder of Emotionally Focused Couples Therapy and the author of Hold Me Tight has trained thousands of therapists on this approach so there are workshops all over! In my experience, couples resonate deeply with this work. The easiest way to find a local workshop is to do a quick search for “hold me tight workshop.” And of course, of course therapy can help immensely too. Focusing your search on therapists who support parents will lead you to the best support for you. Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. It's data time! If you're just tuning in, last year I created an informal survey to collect information about real moms' real emotional experiences with pregnancy and postpartum life. If you're a truth seeker and want these insights sent right to your inbox, sign up here.
Last month I got to sit down "with" Catherine O'Brien of Happy With Baby to talk about my experiences being a mom. You can view it here!
What I love about this project is that by asking numerous moms the same questions and listening, really listening for the answers, we hear a lot of shared experiences. I've said it before, and I'll say it again: The power of "me too" is strong, strong, strong. Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. Six months later and I here I am again with some more data to share from my Getting Real survey.
{To have this information sent straight to your inbox, sign up here. This stunning image/data was the first eye-opening result shared.} I figured maternal mental health awareness month would be a good context in which to share (okay, in keeping with getting real, it was not my intention to take this long, but I'll be starting an #itsallaboutME campaign soon – ME = Managing Expectations. So here we are.) I'll be parceling out information in bite-sized pieces from what I learned from these honest moms' generous sharing. With each tidbit, I will also provide some kind of answer to “what do I do with this information” by way of resources and tools. Oftentimes simply hearing shared struggles melts away some of the weighty self-judgment attached. But also, using our experience to help others builds a sense of meaning and purpose. So if you have any sense of “I wish someone had told me that” please share this info with at least one mama or mama-to-be. One of the essential questions I'm always asking myself is “How can we prepare for and support new moms without scaring the shit out of them”? I invite you into that same line of inquiry, now and forever. Here's a sneak peak at some of what I learned:
Okay, all for now, more soon! As usual, if you or a local San Francisco mama you love needs, support I am here. Other places to search for help from professionals trained specifically in maternal mental health are through PSI and Postpartum Project (this is an awesome newer resource with a database of all kinds of support - from mental health to lactation consultations to doulas and more! Keep checking back as it grows). Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. Your words matter.
To feel depressed or anxious anytime is difficult. To feel this way during a time society says is supposed to be nothing but joyous is devastating. Whether you are the friend, spouse, parent or neighbor of a mom who is struggling while pregnant or after having a baby, or if it's YOU reading this, mama, the way you respond is important. Since the experience of postpartum suffering is like an open wound, the way we treat it can feel like a soothing salve or a stinging squeeze of lemon. (If you cringed at that last sentence, that's it - you already get it!) Sometimes we say the wrong things. It's not for lack of caring. In fact, it's often our way of trying to help. But good intention carries little value if it cannot be absorbed by the very person its intended for. I think it's fair to say we've all been on both sides of this. Since most of us have to fumble through difficult conversations at one time or another, here are some tips on how to talk to a mama who is struggling in a way that will maximize that soothing response. Again, these are just as relevant for how to talk to SELF as for other. When learning mom is having a hard time, thank her from the bottom of your heart for sharing this with you, and then: 1. DO genuinely empathize and reflect how tough that sounds. Accurate empathy calms our nerves.This could sound like: I can imagine how hard it must be to care for such a new and needy person while feeling down. It must be tough to be working so hard and not feeling well. For the mamas reading, go ahead and try to say these soothing statements to yourself and see if they feel different than the usual "if I was a better mom, I wouldn't feel this way in the first place" nonsense. DON'T start any sentence with "but." But look at your baby - he's perfect! But you look great! Yep, baby is doing fine and mom's distress is getting in the way of being able to enjoy him. Mom looks great because she's desperately trying to mask the fact that she feels like shit. While of course you are likely trying to be reassuring, when you respond with "but" it inadvertently invalidates mom's very real experience. 2. DO ask "what can I do to help"? This sends the bold and simple message, "You are not alone. I am here with you." She may feel so terrible about needing help that it's hard to ask for exactly what she needs. She might be so overwhelmed that she doesn't even know. While respecting mama's wishes, you can gently offer some ideas, such as keeping her company, remaining a phone call away, doing some chores around her house (or you can sneak them in while visiting), bringing food, holding the baby while she showers or otherwise tends to herself. For moms reading this, you might ask yourself "what would feel helpful right now. What do I need"? Yes, the answer may be unobtainable at times. (like if you want 10 straight hours of sleep or a trip to Hawaii yesterday), but other times perhaps you'll find you need a hug or a burrito from your favorite spot. DON'T offer a vague, "let me know if I can help." There's a difference between asking "how can I help" (it lends an air of action and willingness) and "let me know if I can help" (it's distant and can lack in sincerity). Again, mama might not ask for help in any way, but at least set her up for real connection with your offer and your self. 3. DO relate to the extent that you can. Only do this if it's genuine. Maybe you had another friend or relative move through a difficult postpartum period, or you're up to date on how common both the baby blues (~ 80% of postpartum moms) and postpartum depression (~15%) and anxiety (~10%) are. Perhaps you suffered yourself (danger zone, see below!). This might sound like: My cousin went through postpartum depression with her first. You're so not alone, a lot of woman struggle in the first year. I had a ton of anxiety when I had my daughter. It sucked, but I got help and it feels like a distant memory now. For mamas reading, tell yourself that many amazing women have been through the same excruciating experience and come out on the other side. Need help? Resources below! DON'T try to one-up this suffering mama with war stories of those you perceive had it "worse." Also don't drop off a simple "everyone feels this way." Sometimes we want mom to think it's not that bad (or we truly don't understand how bad it is), so we either tell her it's normal (it's very common, yes - see stats above - but not normal per se, as in we need to tend to it in order to get to the real normal) and change the subject, or share information that we think will demonstrate how small the problem is. These sentences sometimes start with the words "at least." At least you have a partner. My neighbor raised six kids all alone. At least you aren't that woman on the news last week who . . . The issue here is twofold. Mom already feels like the situation isn't that bad (again, our culture tells us this is the best, most treasured time, even though it's so hard!), but that she is faulty in some way for struggling. This is the voice of depression, and it's neither logical nor loving. Also, we can't compare suffering, as each of us experiences life in a different way, plain and simple (not to mention, you likely know a fraction of the story of your neighbor or women you see on TV). While mom is in the thick of her distress, focus on her and her experience, and believe she feels exactly as bad as she says. Even if you wish she didn't. If you've gone through a similar experience, you may feel compelled to share all the scary thoughts and deep despair you felt. While your story is worthy of attention too, now may not be the time to share each and every detail. There's a fine line between normalizing and oversharing in a way that can be overwhelming. When in doubt, check in with this vulnerable person you're attempting to support to see if what you're sharing is helpful. This could sound like "Would it be helpful to hear a little about my experience and how I got through it"? To be present with your own or someone else's suffering can be hard, as can knowing the right way to respond. Hopefully these tips, which don't have to be perfectly executed can help guide the way. If you are gifted with the knowledge that mom is really struggling and could use some extra help, here are some good things to know. Everything from postpartum depression to anxiety to psychosis is highly treatable. Women can and will feel better again. If you want to learn more, a great starting point is PSI: You can also call their warm line between 9:00 AM – 9:00 PM at 1-800-944-4773. Right here In San Francisco you can call Talkline 24/7: (415) 441-KIDS or (415) 441-5437. They also have in-person services. They. Are. Awesome. And here is a comprehensive list of San Francisco maternal mental health resources: Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call.  Why talk about postpartum mental health? It's thought that about 80% of women experience the “baby blues,” a short term (about two weeks) bout of sad-weepy-moodiness brought on primarily by hormonal shifts. A smaller percentage of women have more serious, but highly treatable, mental health concerns, commonly known as Perinatal Mood and Anxiety Disorders or PMADs. Neither the blues nor the PMADS are openly talked about (yet), likely because we're all walking around believing pregnant women and new moms are meant to be basking in the glow of impending or new motherhood. And there are are amazing, tender, hard-to-put-in-words, heart-bursting pieces of the experience. But, like with anything, pretending the hard parts aren't there when they really are just makes everyone secretly feel like they're doing life wrong, making us even less likely to be honest and open. It's not hard to see how easily the cycle is perpetuated, and the consequences are shitty at best (holding shame and self-judgment) and dangerous at worst (having untreated mental health issues that impact you and your child). So let's get educated first. Later, you get to decide if you would like to be honest about your own experience with those you decide are supportive and deserving of your story. Getting to know the tougher end of the spectrum. Below is information about the most common PMADS. These statistics and symptoms are taken directly from the Postpartum Support International (PSI)'s extremely informative website, edited to fit in one space so you don't have to click around. The links within will take you to more elaboratate descriptions in “plain mama English” on the Postpartum Progress website. More on both of these amazing organizations later. Depression: `Occurs in ~ 15% of postpartum and ~ 10% in pregnant women Perinatal depression is the most common complication of childbirth. Symptoms include:
Anxiety: Occurs in ~ 10% of postpartum and ~ 6% of pregnant women. It may be experienced alone or in conjunction with depression. Symptoms include:
OCD: According to PSI, "Postpartum Obsessive-Compulsive Disorder (OCD) is the most misunderstood and misdiagnosed of the perinatal disorders. You do not have to be diagnosed with OCD to experience these common symptoms of perinatal anxiety. It is estimated that as many as 3-5% of new mothers and some new fathers will experience these symptoms. The repetitive, intrusive images and thoughts are very frightening and can feel like they come “out of the blue.” Research has shown that these images are anxious in nature, not delusional, and have very low risk of being acted upon. It is far more likely that the parent with this symptom takes steps to avoid triggers and avoid what they fear is potential harm to the baby." Symptoms include:
Psychosis: Occurs in ~ 1 to 2/1,000 deliveries, or ~ .1% of births. Onset is typically sudden, usually within the first 2 weeks postpartum. Symptoms include:
Got it. Now what? Okay, now you know the general scoop on these disorders. So what if you notice symptoms in yourself or someone you love? Below are options depending on severity.. You can loosely think about what category you fall into and/or take this valid and reliable depression inventory, which has anxiety items on it as well (this won't screen for other PMADS). Of course, calling me (or abother practicioner in maternal mental health) is a reasonable option regardless of severity, but let's make sure you have the full range of appropriate options. Severe (it's real bad, even if it's hard to admit; score of 19 and above): Call your doctor and let her or him know what's happening for you. Yes, this will be hard. Yes you should do it anyway. There is no perfect time. If you have a hunch that it will help, make the call. *Important Note: Postpartum Psychosis is a medical emergency and needs to be treated right away. This means you need to get to an emergency room ASAP, and once there be real honest about what's happening for you, including all the scary and harmful thoughts. Until you've connected with the appropriate support, you should be accompanied at all times. And remember, as intense as this is, it's treatable. This level of scary won't last forever. Mild-Moderate (this is not normal for you and it's getting in the way of you feeling like yourself*; score of 13-18): Call me or another provider educated/skilled in maternal mental health. The recommended treatment for mild to moderate postpartum depression and/or anxiety is therapy. For moderate – severe, medication is recommended, and there is a variety of other non-medication options as well, such as light therapy and acupuncture. Note: If medication is presented as an option and your first thought is “but I'm breastfeeding,” I'm linking you to two sites that can give you sound information about that. There are some medications considered safe options while breastfeeding, which is good to know even if you decide it's not for you (i.e., you can help spread the word so other mamas don't make uninformed choices!). LactMed is the National Institute of Health's huge inventory of info on the subject and Mind Body Pregnancy is the brainchild of a San Francisco psychiatrist, passionate about getting this information out to the masses. Mild (symptoms are pesky and in the way of feeling like your best self*; score of 10-12): Call me or another provider educated/skilled in maternal mental health and/or create or check in with your personal wellness plan. Are you doing the things that you know work on better days, such as getting movement, talking with trusted friends, resting, eating well, praying, or whatever your specific tools are? Are you letting the helpers help? Do you need different ones? Do a quick assessment and see what you see. Remember, this is the biggest adjustment you've ever made, and it's challenging at its core. Of course feeling well is going to take more effort and resources. *even the concept of feeling like your best self should be taken in the context of adjusting to your new mama self. On Online Resources: Click wisely As you probably know, when it comes to the internet, the line between staying informed and getting overwhelmed is thin. For the sake of your emotional health, I recommend that you, first and foremost, tune in to your inner wisdom or that of someone(s) who knows you well enough to have a fair say in what's happening when your wisdom is overshadowed by overwhelm, self- criticism, sleep deprivation, or simply the hardcore newness of this whole thing. In terms of the web, it's my personal opinion that you focus on the aforementioned online maternal mental health resources. Postpartum Support International is like the kind, giving grandmother of this family, who tells it like it is, without a lot of “extra.” In addition to the basic information provided above, she has answers to your frequently asked questions, a warm line that you can call in times of need (not for use in a medical emergency.), and the numbers for who to call in your city, state, or country to find an appropriate resource. She's the one who teaches many of us clinicians about this work and also offers stories from countless women just like you on the PSI blog. Postpartum Progress is also a wellspring of information, but has more of the tone of your sassy aunt who's like “Oh honey, come here, I got you.” She's super smart and is on a mission to “create healthier families by raising awareness, reducing stigma, providing social support and connecting mothers to help for perinatal mood and anxiety disorders like postpartum depression.” The best way to see all she has to give is by starting here. One of the sweetest offerings is a year's worth of daily hope emails. Of course, of course be open to other resources that are helpful to you. What I caution against is Googling all your symptoms and noticing four hours and 17 chatrooms later that you still aren't quite sure what's happening or what you need. Okay, I think that's enough for now, yes? If you've gotten this far, go ahead and thank yourself for staying informed. It's truly half of the work, mama. Now, go take a nap. xoxo Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. I asked 200+ women to share their honest experiences of pregnancy and the postpartum period.
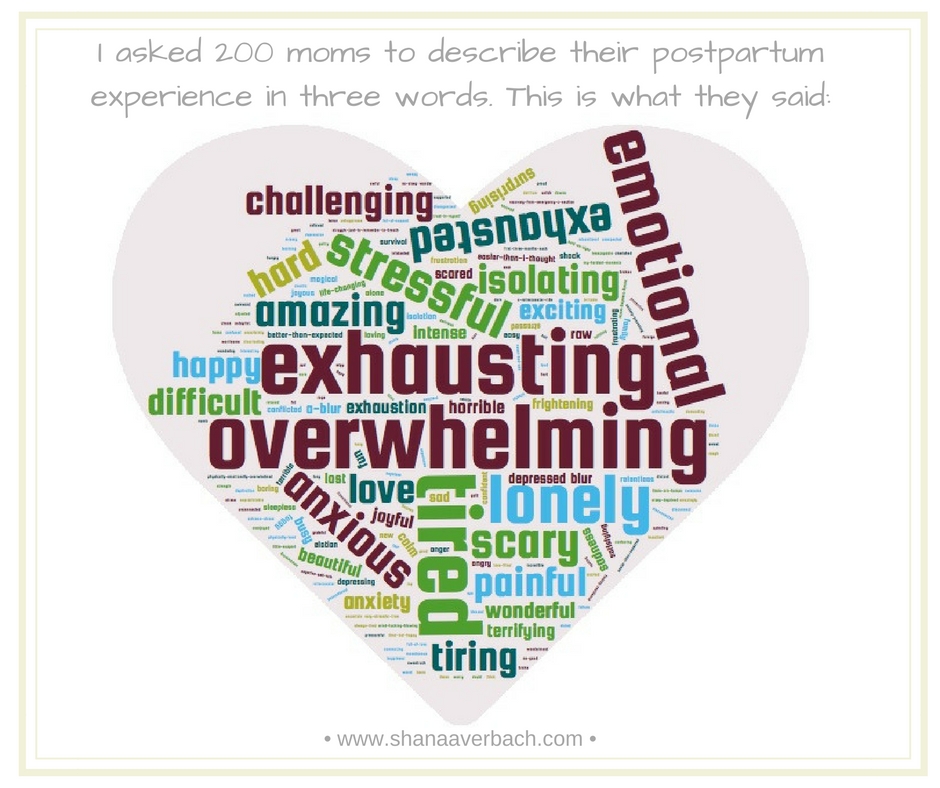
The results are a beautiful collection of raw experience filled with the joys and the difficulties, incuding what you see in the graphic above, which is the collective answer to the question: "What are three words that you would use to describe your postpartum experience"? My next step is analyzing the information, which includes input on thoughts, feelings, supports (or lack thereof), relationship issues, and what women are needing in the way of professional suppor, such as counseling during pregnancy and postpartum, groups, and online support. The heart of my goal is to get real about what this phase of life is like, so that women can start to see that there is so much shared experience - including those things you thought no one else thought or did - and can get the most appropriate type of support, both from professionals and one another. If you want to learn what I learn and stay up to date on info + offerings, sign up here. Yours in wellness, self-care and compassion, Shana Think I may be the right fit for you or a loved one? Feel free to email me at [email protected] or call 415-963-3546 for a free 20-minute consultation call. |
Archives
September 2019
Categories
All
|
| Copyright © Shana Averbach, LMFT 2024. All rights reserved. | 919 Irving Street, Suite 104 San Francisco, CA 94122 | 415.963.3546 | San Francisco Therapy, Counseling, and Resources for Women - Pregnancy Support, Motherhood, Postpartum Adjustment |




 RSS Feed
RSS Feed